With recent announcements in the National Health Service (NHS) 10-Year Health Plan for England, the UK government has affirmed its commitments to reduce NHS wait times and improve patient care, for example, by using robot-assisted surgery. National Institute for Health and Care Excellence (NICE) guidelines identify six systems for orthopaedic surgery and five systems for soft tissue procedures as part of an evidence generation plan spanning three years.
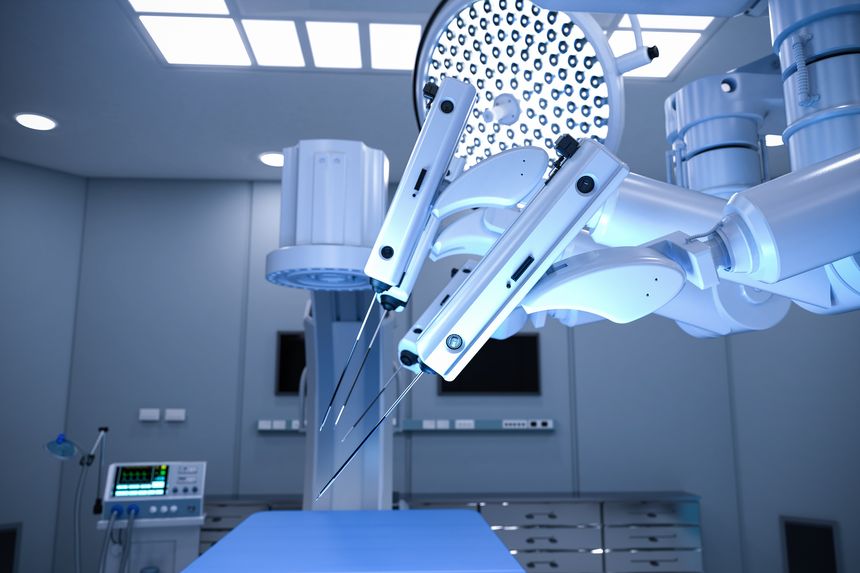
Robotic surgical systems generally comprise wristed robotic limbs which can be used to hold implements or manipulate tissue, guided by a camera. Semi-active systems will also provide the surgeon with haptic feedback which helps to prevent injury to the patient. Many of these systems have a short learning curve for the surgeons operating the system, and are less physically taxing to use compared to traditional surgery, which may enable a surgeon to carry out more surgeries in a given day. However, on balance, robot-assisted surgery is associated with longer set-up times in operating theatres and high start-up costs.
Investment in robotic surgical systems has the potential to invigorate the NHS. However, it is equally important to consider the infrastructure, including clinician training, which surrounds this technology. As recently as October 2025, Intuitive Surgical opened the UK’s largest training centre for robot-assisted surgery (RAS) in Reading, following a track record of supporting 89,000 surgeons globally in RAS training. The da Vinci SP, da Vinci X and da Vinci Xi (Intuitive Surgical Systems) have all been approved by NICE for soft tissue procedures.
Focusing on prostatectomies, a recent case study based on NHS surgical statistics observed that robot-assisted surgery reduced patients’ length of stay by 50%, with increases in hospital productivity. In a handful of UK cases, patients undergoing a robot-assisted radical prostatectomy have been able to return home the same day as their surgery. Robot-assisted surgery also allows clinicians to further personalise the surgical techniques to each patient, such as personalised knee replacements being carried out at Ysbyty Gwynedd hospital, Wales.
Robot-assisted surgery is becoming well-established for treating adults in the UK. However, robot-assisted paediatric surgery is also gaining traction. In February 2025, the Versius Surgical System was used in a robotic pyeloplasty procedure to treat a four-month-old baby’s narrow ureter – at the time, the world’s youngest Versius patient. The system’s precise, 5 mm instruments enable surgeons to reduce the size of surgical incisions and minimise blood loss, accelerating patient recovery times.
Beyond the UK, at Johns Hopkins department of paediatric oncology, transoral robotic surgery is used on babies as soon as two weeks after birth to treat conditions such as refractory sleep apnea, vascular malformations, cysts, and conditions affecting the larynx. Research at Johns Hopkins also extends to AI-assisted surgery, such as gall bladder removal carried out on pigs.
These cutting-edge procedures demonstrate the flexibility of robotic surgical systems. Recent trials suggest that in the future, world-leading surgeons will be able to operate wherever they are needed most, through telesurgery. A major milestone in telesurgery was achieved in November 2025 by Professor Iris Grunwald and Ricardo Hanel, who were involved in the world’s first transatlantic remote thrombectomy.
In their recommendations for soft tissue procedures, NICE noted that minimally invasive surgery is performed less frequently in more deprived areas of the UK. The UK government have announced plans to establish national registries for robotic surgery data and develop telesurgery networks from 2029, which may help to alleviate the disparity of care across the UK.
Innovations in robotic surgery are not limited to applications of the systems. In contrast, research institutions, medical device companies, and even health boards and hospitals are continuously pioneering new robotic surgical systems.
CardioPrecision is a spinout of InnoScot Health, NHS Greater Glasgow and Clyde, and the Golden Jubilee National Hospital. Their patented CoreVista® Robot Enabling Platform has been used in robotic transcervical aortic valve replacement (AVR) throughout Scotland. AVR is an alternative to open heart surgery, requiring only four small incisions.
Robotic surgery in the brain also promises a shift away from traditional techniques towards devices which can deftly navigate inside the brain. Robeauté hold a US patent for a “System and Method for Real-time Localization” related to their microrobot intended for neurosurgery. As an alternative to rigid electrodes, the microrobot is designed to manoeuvre by elongation and contraction along a path mapped out by the neurosurgeon in an attempt to preserve brain tissue and minimise damage.
Researchers at Southern Methodist University and George Washington University have developed microrobots controlled using magnetic fields, with a so-called “magnetic tweezer system.” Another approach is the Symphony Robotics flexible micro-robotic arm involved in a collaboration with Monteris Medical to treat brain tumours and drug-resistant epilepsy.
The landscape of robotic surgical systems is constantly evolving. UK trials intended to help understand surgeon experience and clinical impact have the potential to improve patient outcomes across thousands of surgeries. Increased investment, adoption, and education surrounding these systems will provide new opportunities for excellent patient care, in the UK’s National Health Service and beyond.
Marks & Clerk have a host of clients working in this space and have a large team of patent attorneys with specialist knowledge to support these clients and ensure they obtain the best possible protection for these transformative and life-saving innovations.


/Passle/6130aaa9400fb30e400b709a/SearchServiceImages/2026-03-06-21-46-38-285-69ab4b3e33137c4539672718.jpg)
/Passle/6130aaa9400fb30e400b709a/SearchServiceImages/2026-03-06-21-19-43-810-69ab44ef33137c4539671856.jpg)
/Passle/6130aaa9400fb30e400b709a/SearchServiceImages/2026-03-05-11-36-51-736-69a96ad3535084dd60cc14f1.jpg)